VRE
As of March 2, 2026, there are no outbreaks of VRE bacteremia at Bruyère.
At Bruyère, we take our patient care and safety very seriously, and we are committed to transparency. On a quarterly basis, since December 2008, we have been reporting Vancomycin-resistant Enterococcus bacteremia (VRE bacteremia) rates at our two hospitals (Bruyère Health Élisabeth-Bruyère Hospital and Bruyère Health Saint-Vincent Hospital) on our website. The analysis of our VRE bacteremia rates over time will provide us with valuable information that we will use to improve quality of care in our organization.
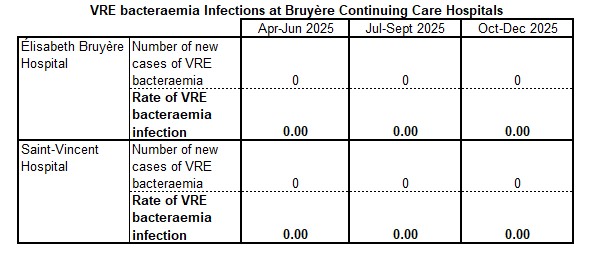
Rates of VRE bacteremia are one of a number of patient safety indicators that all Ontario hospitals publicly report. These indicators are posted on the Health Quality Ontario website.
Public reporting of VRE bacteremia rates is not intended to serve as a measure to compare hospitals against each other. First of all, it is important to remember that rates at most hospitals will vary from month to month. Furthermore, it is important to take into account the specialty care within the various facilities, implying different risk factors. Thus, when considering hospital performance, it is essential that VRE bacteremia rates be viewed in the context of other performance indicators.
VRE Q&A
Have more questions? Email us
Q: What is Vancomycin-resistant Enterococcus (VRE)?
A: Enterococci are bacteria that live in the gastrointestinal tract of most individuals and generally do not cause harm (this is called “colonization”). Vancomycin-resistant enterococci (VRE) are strains of enterococci that are resistant to the antibiotic Vancomycin. If a person has an infection caused by VRE, such as a urinary tract infection or blood infection, it may be more difficult to treat.
Top
Q: What is bacteremia?
A: Bacteremia is the presence of bacteria in the bloodstream and is referred to as a bloodstream infection. Accompanying symptoms could include a rise or a drop in body temperature, change in mental or functional status, and a change in blood pressure.
Top
Q: What is a case of VRE bacteremia?
A: A patient who is identified with laboratory confirmed bloodstream infection with Vancomycin-resistant Enterococcus (VRE).
Top
Q: What are healthcare-associated infections?
A: Sometimes when patients are admitted to the hospital, they can get infections. These are called healthcare-associated infections. This may mean that certain symptoms began 72 hours after admission to the hospital; or that the infection was present at the time of admission, but was related to a previous admission to that hospital within the last four weeks.
Top
Q: What are the risk factors for VRE infection?
A: People at risk for colonization or infection with VRE are usually hospitalized and have an underlying medical condition, which makes them susceptible to infection. These conditions include patients with:
- Recent hospitalization in health care facilities outside Canada
- Critical illness(es) in intensive care units
- Severe underlying disease or weakened immune systems
- Urinary catheters
- Exposure to (or contact with) a patient with VRE
- Antibiotic use, particularly vancomycin
Top
Q: How is a VRE bacteremia treated?
A: Treatment with specific antibiotics is required.
Top
Q: How is VRE spread?
A: VRE is spread from one person to another by contact, usually on the hands of caregivers. VRE can be present on the caregiver’s hands either from touching contaminated material excreted by the infected person or from touching articles soiled by feces.
VRE can survive well on hands and can survive for weeks on inanimate objects such as toilet seats, taps, door handles, bedrails, furniture and bedpans. VRE is easy to kill with proper use of disinfectants, and good hand hygiene will eliminate the bacteria from contaminated hands.
Top
Q: How does Bruyère control the spread of VRE?
A: Good hand hygiene, i.e. washing hands thoroughly and often, is the single-most effective way to prevent the spread of infectious diseases like VRE.
Good Hand Hygiene Practices include washing your hands:
- After using the bathroom
- After blowing your nose
- Before eating and drinking
- Before and after you have contact with dressing or wounds
- When your hands are visibly soiled
- Before you leave your room
Remind all staff and visitors to practice good hand hygiene before and after they take care of you. Ask your nurse or doctor to demonstrate proper hand hygiene [15 seconds of soap and running water OR waterless alcohol hand rub (such as Purell) until hands are dry].
Top
Q: What is Care doing to improve patient safety?
A: We have a patient safety program in the hospital to make sure that all practices are at the highest level possible to keep you safe. This includes:
- Ensuring that our housekeeping practices are in line with the best practices in healthcare
- Developing a program for excellence in hand hygiene
- Conducting audits on various practices to verify that patient care is as safe as possible
Top